Daily Insulin Use
Insulin use in the United States is very common. Since diabetes may affect any age group, children and adults use insulin. Administered in the fat layer of skin (often in the abdomen, thigh, hip, or forearm), injections are easy to learn to give. Some pharmacies provide them pre-packaged. With sharp, short needles, injections are almost painless. The length of the needle keeps the risk of injecting into a vein minimal and helps to keep the process simple to learn. All you need to do is clean the injection site with alcohol, stick in the needle, and push the plunger.
Here’s the thing, though—Insulin is a potent medication and commands a lot of respect. Therefore, I think it’s vital that you understand some of the basic principles and rules for its administration –to be safe.
How Insulin Works
The drug insulin’s job is to imitate the body insulin’s actions produced by the pancreas. The pancreas produces a constant amount of insulin that balances liver glucose production with glucose use to maintain normal glucose levels between meals. The pancreas also produces extra insulin during meals to prevent spikes of elevated blood glucose after meals. The amounts produced at such times vary among individuals. Furthermore, insulin production increases whenever an individual has an illness, extreme stress, an infection, or takes medication that may artificially increase glucose levels.
Facts About Insulin
Blood Glucose Values

Timing Insulin Injections
There are four primary types of insulin injections, and each peak lasts different lengths of time. Therefore, you must know when your medication will peak and how long it lasts to manage your blood sugar levels effectively.
| Type of Insulin | Starts Working | When It Peaks | How Long It Lasts | ||
| Rapid-Acting Insulins | 15 minutes | 30 minutes to 1 hour or 1 1-1/2 hour | no longer than five hours at most | ||
| Short-Acting Insulins | 30 minutes | around two hours and thirty minutes up till five hours | last anywhere from five to twelve hours | ||
| Intermediate-Acting Insulins | an hour after you take them, although some start as soon as 15 minutes, and some wait as late as five hours | from one hour to fourteen though the average seems to be in the four hours to the fourteen-hour range | between 10 to twenty-four hours | ||
| Long-Acting Insulins | one hour but no later than four hours | Six and twelve hours | up to twenty-four though some last as long as forty-two |
Factors Affecting Absorption
- There are multiple injection sites available for giving an insulin injection. Where you choose to insert the needle can change the insulin absorption speed. You can find the best sites for absorption in the abdomen and two inches around the navel.
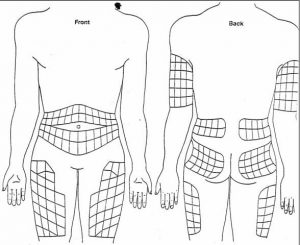
- Rotate Injections sites daily to allow them to heal before reusing them. For absorption to work best, use one area of the body at a time, and move through each possible injection site before moving to a new area of the body. Staying in the same body area provides greater consistency in the absorption rate.
- Don’t use heat or massage (rub) to help speed up the absorption time. The opposite is true as well; don’t apply ice to slow it down.
- Base the timing of when you take your insulin and when you eat on how rapidly your insulin acts. For instance, take fast-acting insulin about ten minutes before a meal if your blood sugar remains within a normal range. On the other hand, give regular insulin between twenty to thirty minutes before a meal since the effect occurs slightly slower.
Ignatavicius, Donna D., M. Linda Workman, Cherie R. Rebar, Nichole M. Heimgartner. Medical-Surgical Nursing> Concepts for Interprofessional Collaborative Care. (2018) 9th Ed. St. Louis: Elsevier. ((1294)
Self-Monitoring Blood Glucose
- Knowing your blood glucose levels helps you determine if and how you might need to adjust your diet or your insulin dose to prevent episodes of extremely high or low blood sugars. Being able to keep blood glucose within a healthy range helps to reduce the risks of complications of diabetes and improves overall health and well-being.
- Know how to work your monitoring device correctly. Follow the manufacturer’s instructions and use the test strips designated for the specific monitor.
- Do not reuse or use expired strips.
- Remember to change the test strip code in your monitor to match the new strips when you purchase a new package of test strips.
- Regularly do quality control tests of your trips to make sure you are getting accurate test results.
- Follow proper hand hygiene before testing your finger.
- Make sure you have a good blood drop sample to do the test.
- Clean the monitor thoroughly to remove any dried blood from the testing area.
Ignatavicius, Donna D., M. Linda Workman, Cherie R. Rebar, Nichole M. Heimgartner. Medical-Surgical Nursing> Concepts for Interprofessional Collaborative Care. (2018) 9th Ed. St. Louis: Elsevier. ((1296)
Hypoglycemia- Low Blood Sugar
Once blood glucose levels drop below 70 mg/dL, blood sugar levels unstable are unstable. If your body responds as it should, the liver begins to release glycogen, and protein breaks down into glucose. If that chain of events doesn’t move along as it should, then life-threatening hypoglycemia may develop.
Symptoms of hypoglycemia are different among people in that abnormal blood glucose levels and hypoglycemia can exist separate from each other. Therefore, it’s important to go by the symptom and not the blood sugar reading on the glucose monitor when deciding whether to head to the emergency room for treatment.
Here is a list of low blood sugar reactions. A person may experience only a few or a lot of them.
- Weakness
- Shaky/tremulous
- Sweaty
- Fatigue
- Heart-Pounding
- Hungry
- Difficulty Thinking
- Nervous/Anxious
- Tingling
- Confusion
- Behavior Changes
- Emotional Instability
- Seizures
- Loss of Consciousness
- Brain Damage
- Death
Insulin Storage
- Store extra bottles (vials) of insulin in the refrigerator. Do not store them in the freezer.
- Keep vials out of direct sunlight.
- Refrigerated insulin may be uncomfortable when used as an injection. Therefore, you may keep the insulin vial currently in use out of the refrigerator at room temperature but out of direct sunlight for up to 28 days. Discard any remaining medication after 28 days.
- Don’t shake the vials to mix them; instead, roll them between your palms. Discard the medication if it becomes cloudy or clumps together.
- Prefilled syringes remain stable for 30 days if stored in an upright position (needles pointing up) in the refrigerator.
Ignatavicius, Donna D., M. Linda Workman, Cherie R. Rebar, Nichole M. Heimgartner. Medical-Surgical Nursing> Concepts for Interprofessional Collaborative Care. (2018) 9th Ed. St. Louis: Elsevier. ((1297)